Empowering patients by highlighting the treatment pathways for UI & FI
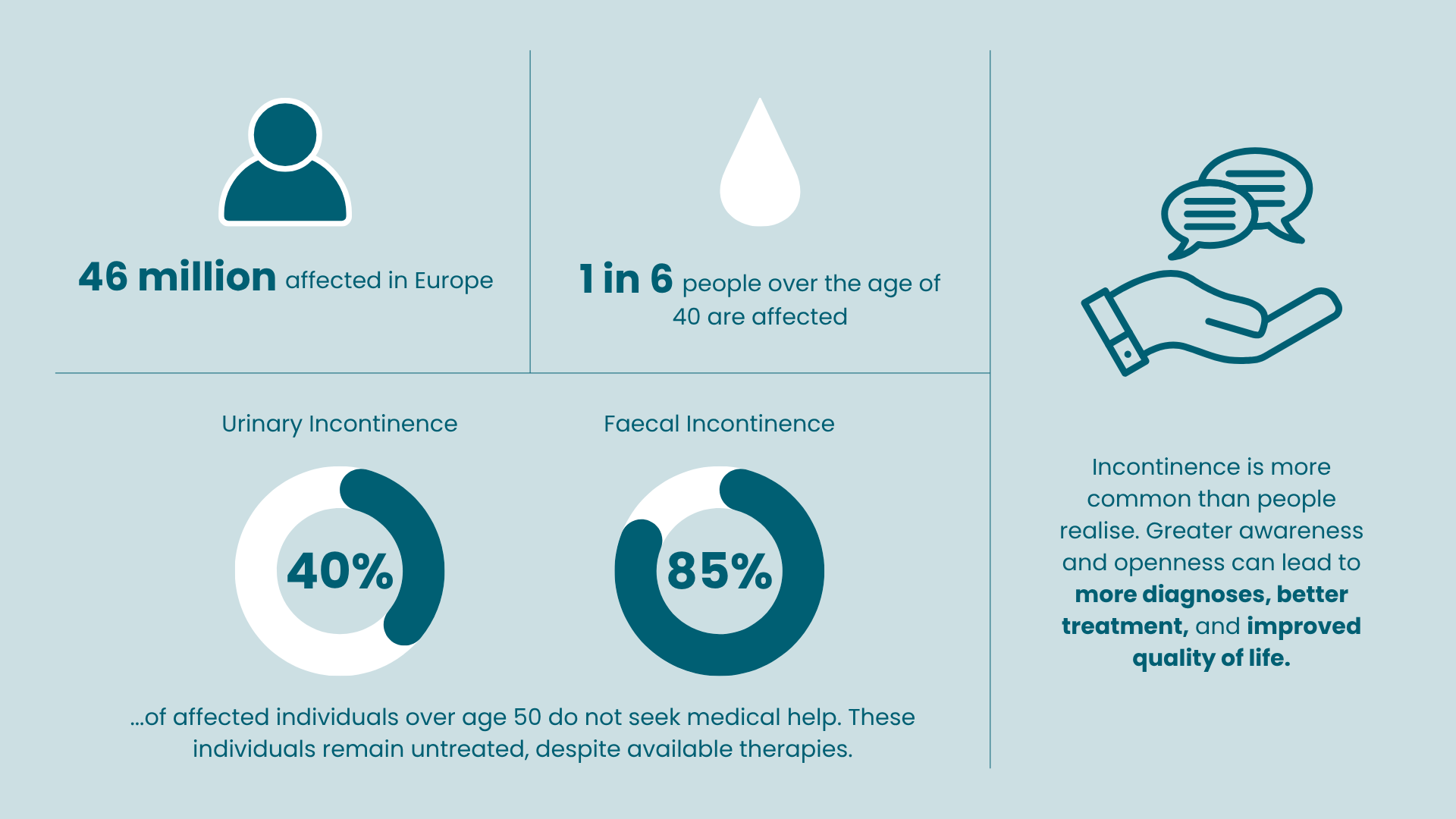
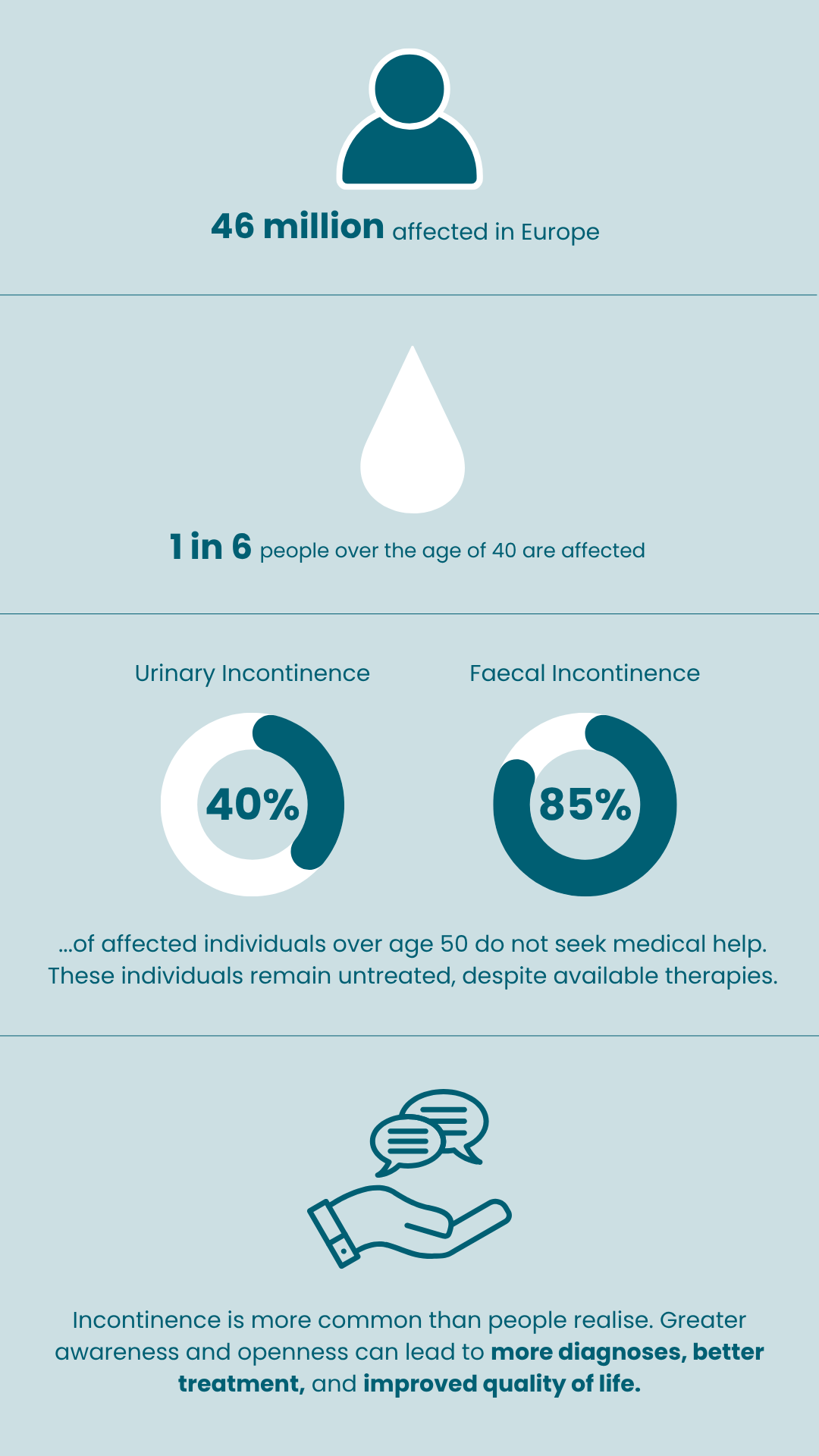
Doctors distinguish between two types of incontinence: urinary and faecal. Both are serious issues that can greatly affect a person’s quality of life, sometimes leading to feelings of isolation from others. In fact, about on in six people over the age of 40 in Europe are affected, which adds up to around 46 million individuals.
Unfortunately, incontinence is often seen as a taboo topic. Around 40% of people over 50 with urinary incontinence do not seek help, meaning they go untreated. For those with faecal incontinence, the numbers are even higher, with about 85% choosing not to seek medical assistance.
To find out more.
Select the Urinary Incontinence or Faecal Incontinence tab below
What is Urinary incontinence (UI)
Bladder control problems can be treated, and there are ways to manage the symptoms. Many people mistakenly think that losing control of urine is just a normal part of getting older or something that happens after having a baby. However, it is actually a medical issue that should be discussed with a doctor. It’s important to seek help if you’re facing these challenges.

Urinary incontinence treatment options
If you’re dealing with issues like frequent urges to go to the bathroom or unexpected leaks, the good news is that there are ways to treat these problems. While using pads and other simple solutions can help, they might not fix the underlying issues causing your symptoms. There are more options out there that can provide better relief.
Behavioural treatments
There are several lifestyle changes and simple actions you can take to help manage urinary incontinence. Here are a few suggestions that might make a difference:
- Weight loss/maintaining a healthy weight
- Reducing the intake of stimulants (e.g. caffeine, theine, alcohol)
- Maintain an appropriate level of hydration
- Keeping a bladder diary on paper (some hospitals also offer digital tools, such as the Minze Diary Pod).
- Perform bladder training
Kegel exercises can help strengthen the muscles under the uterus, bladder and large intestine. They can help men and women who experience problems with urinary leakage or bow el control.

Hypopressive abdominal gymnastics involves working on the abdominal region using breathing techniques based on expiratory apnea.


Medication
Medications can be useful for treating different types of incontinence, which is when someone has trouble controlling their bladder. However, it’s important to know that these medicines might come with some unwanted effects.
- Anticholinergics or beta-3 agonists for urinary incontinence.
- Antibiotics for urinary tract infections.
- Oestrogen therapy for mild forms of stress incontinence.

Surgical therapies
Surgery might be necessary if other treatment methods aren’t effective. Some options for surgery include:
For stress incontinence: slings made of a surgical mesh that restore the normal anatomy of the bladder.
For overactive bladder symptoms:
Botulinum toxin A (Botox) injections every six months which are used to reduce bladder contractions by acting on nerve endings in the bladder wall
Sacral Neuromodulation (SNM): SNM provides continuous stimulation of the sacral nerves, using low-amplitude electrical impulses to restore control of bladder functions. Read more about the Sacral Neuromodulation therapy

Downloads
Urinary incontinence myths Vs facts

Myth
Incontinence is a normal part of aging.
Fact
While UI is more common with age, it is not inevitable. It often has treatable underlying causes, and many older adults remain continent with proper care and treatment.

Myth
Only women experience urinary incontinence.
Fact
Although women are more likely to experience UI due to childbirth and hormonal changes, men can also develop UI, especially due to prostate issues or surgery.

Myth
If you drink less water, you’ll leak less.
Fact
Reducing fluid intake can actually worsen UI by concentrating urine and irritating the bladder. Staying hydrated is important for bladder health.

Myth
UI is only caused by weak pelvic floor muscles.
Fact
Pelvic floor weakness is one factor, but neurological disorders, medications, infections, and lifestyle also play a role. Not all cases are about muscle strength alone.

Myth
There’s nothing you can do — just use pads.
Fact
Many effective treatments exist, from pelvic floor therapy and medication to surgical options like sacral neuromodulation or bladder Botox. Pads are not the only solution.
Empowering patients by highlighting the treatment pathways for UI & FI
Clinicians differentiate between urinary and faecal incontinence. This is a serious disorder that can severely limit the quality of life of those affected and may even lead to social isolation. One in six people over the age of 40 is affected, for a total of 46 million people in Europe. 1,2
Incontinence is a taboo subject: around 40 % of all those affected with urinary incontinence 3 above the age of 50 do not seek medical help and remain untreated. For faecal incontinence, the figure is as high as 85 %. 4
1. Milsom, I. et al. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 87, 760 – 6 (20 01).
2. Eurostat Data Explorer for EU28:
https://ec.europa.eu/eurostat/data/database.
International Consultation on Incontinence, Tokyo, 2016.
3. Sullivan R et al: Unreported urinary incontinence: population-based prevalence and factors associated with non-reporting of symptoms in community-dwelling people ≥ 50 years. European Geriatric Medicine, 07 Oct 2020,
12(2):405-412.
4. Damon, H. et al. Prevalence of anal incontinence in adults and impact on quality-of-life. Gastroenterol. Clin. Biol. 30, 37–43 (2006).