Uncovering pathways in bladder and bowel continence care
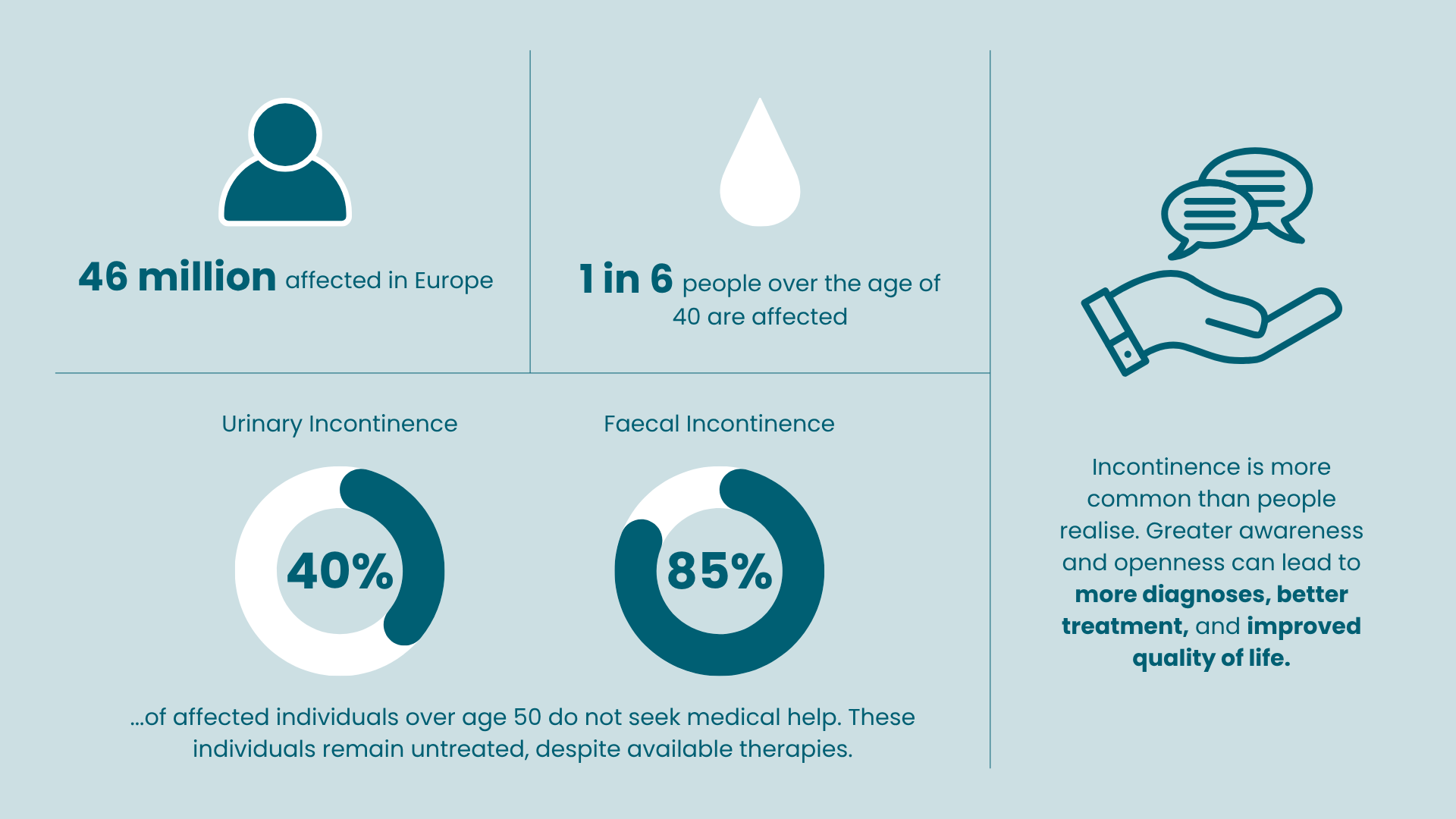
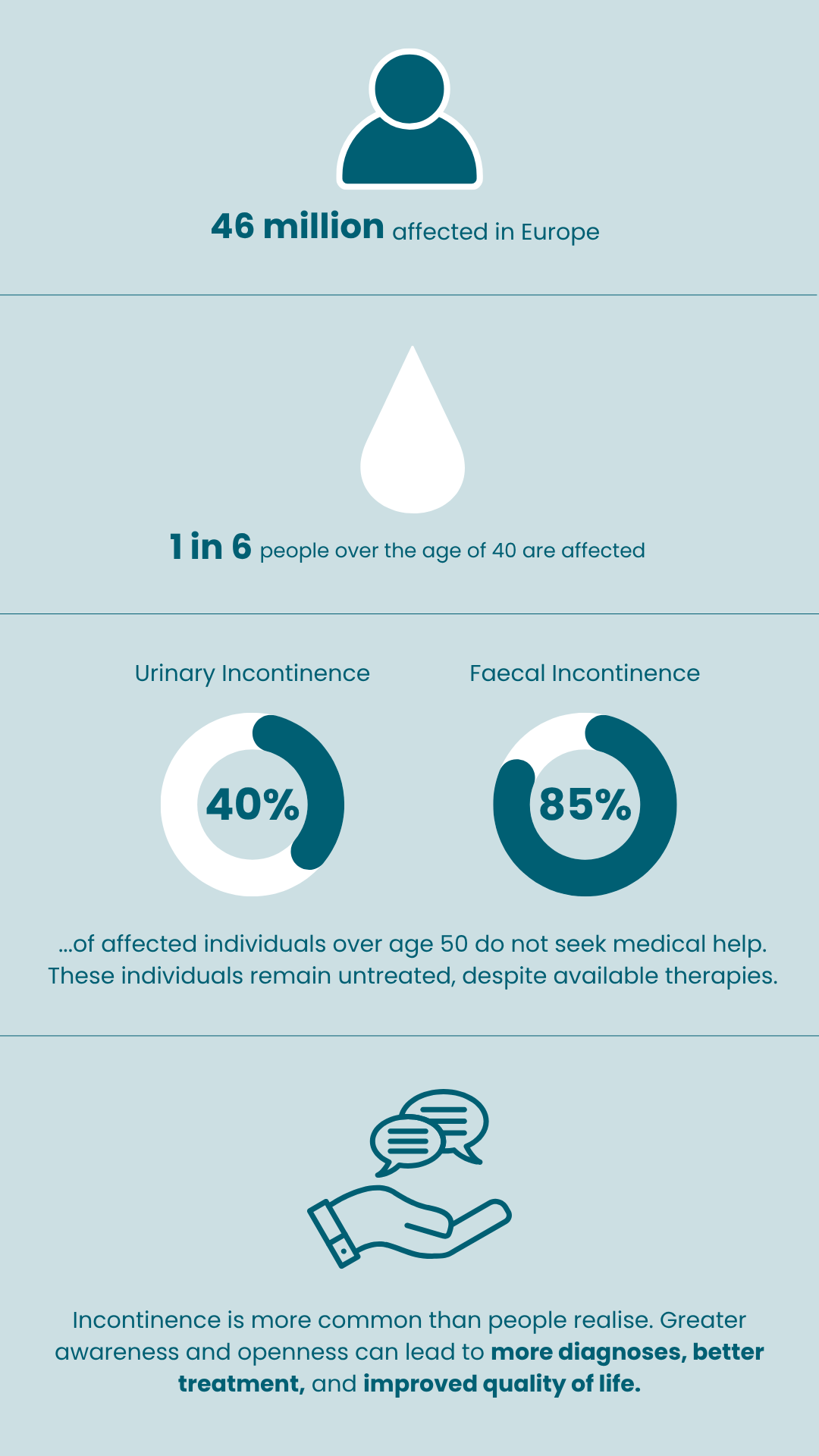
Urinary and faecal incontinence are more common than you might think, affecting around 46 million people in Europe. Unfortunately, many struggle to discuss these issues; over 40% of those with urinary incontinence and up to 85% with faecal incontinence do not seek help.
We believe everyone deserves to live confidently and comfortably. This website offers clear information and resources to help you understand your symptoms and explore treatment options at your own pace.
Choose your path to better care
Select Urinary or Faecal Incontinence to get tailored support and resources.
What is Urinary incontinence (UI)
Urinary incontinence is an uncontrolled loss of any amount of urine from the bladder. It can affect anyone at any age or stage of life. Bladder control problems can be treated, and there are ways to manage the symptoms.
Many people mistakenly think that losing control of urine is just a normal part of getting older or something that happens after having a baby. However, it is actually a medical issue that should be discussed with a doctor.
It’s important to seek help if you’re facing these challenges below.
Assessment
A healthcare professional will undertake a full assessment of your bladder symptoms or refer you to another service for this to be completed. This will include a variety of questions, and you may be asked to complete a bladder diary to see how much urine you pass, how often you are passing urine, and how much fluid you are drinking.
You may also be offered:
A physical examination to see how well your pelvic floor is working.
A urine test.
Asked to complete a quality of life questionnaire to see how much your symptoms are affecting you.
Asked to complete a quality of life questionnaire to see how much your symptoms are affecting you.
The assessment aims to work out what is causing the problems so that you can be offered the treatment that is most likely to work for you.
A doctor should be able to offer initial advice, but may also refer you to other services such as a community bladder and bowel service, pelvic health specialist or hospital services such as urology or urogynaecology.
Urinary incontinence treatment options
If you’re dealing with issues like having to go to the bathroom often or suddenly, the good news is that there are ways to treat these problems. While using pads and other simple solutions can help, they might not fix the underlying issues causing your symptoms. There are more options out there that can provide better relief.
Firstline treatment options:
There are several simple actions you can take to help manage urinary incontinence. Here are a few suggestions that might make a difference:
- Trying to keep to a healthy weight.
- Avoid or reduce drinks containing caffeine (coffee, tea, hot chocolate, cola and energy drinks) or alcohol.
- Drink plenty of water based drinks to stay well hydrated.
- Bladder training.
- Pelvic floor exercise. Women with stress or mixed urinary incontinence may be offered support with learning to do these from a healthcare professional.
Medication
- Medicines that help the bladder to relax and can therefore stop or reduce sudden, strong need to pass urine.
- Antibiotics can be used to treat urinary tract infections.
- Oestrogen (female hormone) creams can be used to treat some forms of mild stress incontinence in women.
When firstline treatments do not help:
Minimally invasive procedures
Other treatment options may be considered for people who have tried initial treatments or for whom the firstline treatments are not suitable. Surgery may be an option for some people. If this is being considered, then a healthcare professional should discuss with you what options are available and the possible benefits, as well as any risks involved.
Botulinum toxin A (Botox)
Injections may help reduce the contractions (tightening) of the bladder wall muscles that can cause sudden and frequent need to pass urine. A healthcare professional will also discuss self catheterisation.
Urethral bulking injections
Involves injecting a gel around the top of the urethra (the tube that urine comes out of), near the bladder.
This helps the urethra to close and reduces urine leakage.
Percutaneous posterior tibial nerve stimulations
Involves having a fine needle put into the skin near the ankle for about 30 minutes weekly, usually for about 12 weeks. This can help some people with sudden and frequent needs to pass urine.
Sacral nerve stimulation (SNS)
Sacral nerve stimulation is used to treat overactive bladder, including urinary urge incontinence and/or urgency frequency and is offered to those unresponsive to other therapies. It
uses low-intensity electrical currents to stimulate sacral nerves, which control urinary functions. The treatment is reversible and can be tested by the patient.
Urinary incontinence myths Vs facts

Myth
Incontinence is a normal part of ageing.
Fact
While UI is more common with age, it is not inevitable. It often has treatable underlying causes, and many older adults remain continent with proper care and treatment.

Myth
Only women experience urinary incontinence.
Fact
Although women are more likely to experience UI due to childbirth and hormonal changes, men can also develop UI, especially due to prostate issues or surgery.

Myth
If you drink less water, you’ll leak less.
Fact
Reducing fluid intake can actually worsen UI by concentrating urine and irritating the bladder. Staying hydrated is important for bladder health.

Myth
UI is only caused by weak pelvic floor muscles.
Fact
Pelvic floor weakness is one factor, but neurological disorders, medications, infections, and lifestyle also play a role. Not all cases are about muscle strength alone.

Myth
There’s nothing you can do — just use pads.
Fact
Many effective treatments exist, from pelvic floor therapy and medication to surgical options like sacral neuromodulation or bladder Botox. Pads are not the only solution.
Downloads
Download this patient pathway flyer for a quick overview of symptoms and treatment options. It can be helpful for discussing symptoms and treatments with a healthcare provider.
Use this worksheet to reflect on your symptoms and treatment priorities. Bring it to your next appointment to discuss the treatment options with a healthcare professional.
Download the interactive Patient Decision Aid for overactive bladder (OAB). Use it to explore your treatment options and find what feels right for you. You can bring this to a doctor to talk about your choices.
Your Health, Your Voice
Incontinence is more common than you might think—and you’re not alone. Our downloadable resources are here to help you better understand your symptoms, explore treatment options, and prepare for meaningful conversations with a healthcare professional.
Feel empowered to be involved in your care. These tools are designed to support open, informed discussions with a doctor, helping you take positive steps towards your health and wellbeing.
Please complete the feedback form and let us know your thoughts.